Introduction
Graves’ disease is an autoimmune disorder that affects the thyroid, a small gland located in the front of the neck. This condition causes the thyroid to produce excess thyroid hormone, leading to hyperthyroidism. Recognizing the early symptoms of Graves’ disease is crucial because early diagnosis and treatment can significantly improve health outcomes and prevent complications. This blog post will delve into the early signs of Graves’ disease, what causes it, how it’s diagnosed, and how it can be managed.
What is Graves’ Disease?
Graves’ disease is a condition that results from an overactive thyroid, which produces too much thyroid hormone. This condition is classified as an autoimmune disorder because the immune system mistakenly attacks the thyroid, leading to an increase in thyroid hormone production.
Importance of Early Detection
The symptoms of Graves’ disease can often be mistaken for other conditions, such as anxiety, stress, or even menopause. This makes early detection challenging, but also highly important. If left untreated, Graves’ disease can cause long-term complications like osteoporosis, heart disease, and even a potentially life-threatening condition called a thyroid storm.
Graves’ disease primarily affects women under the age of 40, though it can occur in men as well. Early detection can lead to more effective treatments and a reduction in the severity of the symptoms.
What Causes Graves’ Disease?
Graves’ disease occurs when the immune system produces antibodies called thyroid-stimulating immunoglobulins (TSIs). These antibodies attach themselves to the thyroid gland and stimulate it to produce excessive amounts of thyroid hormones. Although the exact cause of Graves’ disease is not fully understood, several factors can increase the likelihood of developing this condition.
Is Graves’ Disease an Autoimmune Disorder?
Yes, Graves’ disease is an autoimmune disorder. In autoimmune diseases, the immune system, which usually protects the body from infections and other harmful agents, mistakenly attacks its tissues and organs. In Graves’ disease, the immune system targets the thyroid gland, causing it to become overactive. This results in the production of more thyroid hormones than the body needs.
Common Risk Factors for Graves’ Disease
- Genetics: Having a family history of Graves’ disease or other autoimmune disorders increases the risk.
- Gender: Women are more likely to develop Graves’ disease than men.
- Age: Graves’ disease most commonly affects people under the age of 40.
- Stress: Emotional or physical stress may trigger the onset of Graves’ disease in some individuals.
- Smoking: Smokers, particularly those who have a genetic predisposition to autoimmune disorders, are at a higher risk of developing Graves’ disease.
Environmental Triggers
Certain environmental factors, such as viral infections, can trigger the immune system to attack the thyroid, leading to Graves’ disease. Smoking is also a significant trigger, as it increases the risk of Graves’ ophthalmopathy, a condition where the eyes are affected by Graves’ disease.
Early Symptoms of Graves’ Disease
Spotting the early symptoms of Graves’ disease can be tricky, as they often overlap with other conditions. However, there are some key symptoms to watch out for that can indicate the onset of this autoimmune disorder.
What are the Early Symptoms of Graves’ Disease?
- Fatigue and Muscle Weakness: Feeling unusually tired or weak, even after mild exertion, is a common early sign.
- Unexplained Weight Loss: Despite eating normally or even more than usual, individuals with Graves’ disease often lose weight due to an overactive thyroid.
- Nervousness and Irritability: Increased irritability, anxiety, or restlessness are common symptoms due to the excess production of thyroid hormones.
- Heart Palpitations: A rapid or irregular heartbeat is one of the more alarming early signs.
- Tremors: Shaking or trembling of the hands or fingers can occur, especially in moments of stress or anxiety.
How to Recognize the Signs of an Overactive Thyroid
Graves’ disease is closely associated with hyperthyroidism, where the thyroid gland produces too much thyroid hormone. Here are some key indicators:
- Increased Sweating: Hyperthyroidism leads to a heightened sensitivity to heat, causing excessive sweating.
- Rapid Heart Rate: Individuals often experience an increased heart rate, even while resting.
- Heat Sensitivity: People with Graves’ disease tend to feel unusually warm, even in cooler environments.
Changes in Appearance
Graves’ disease can also affect an individual’s appearance:
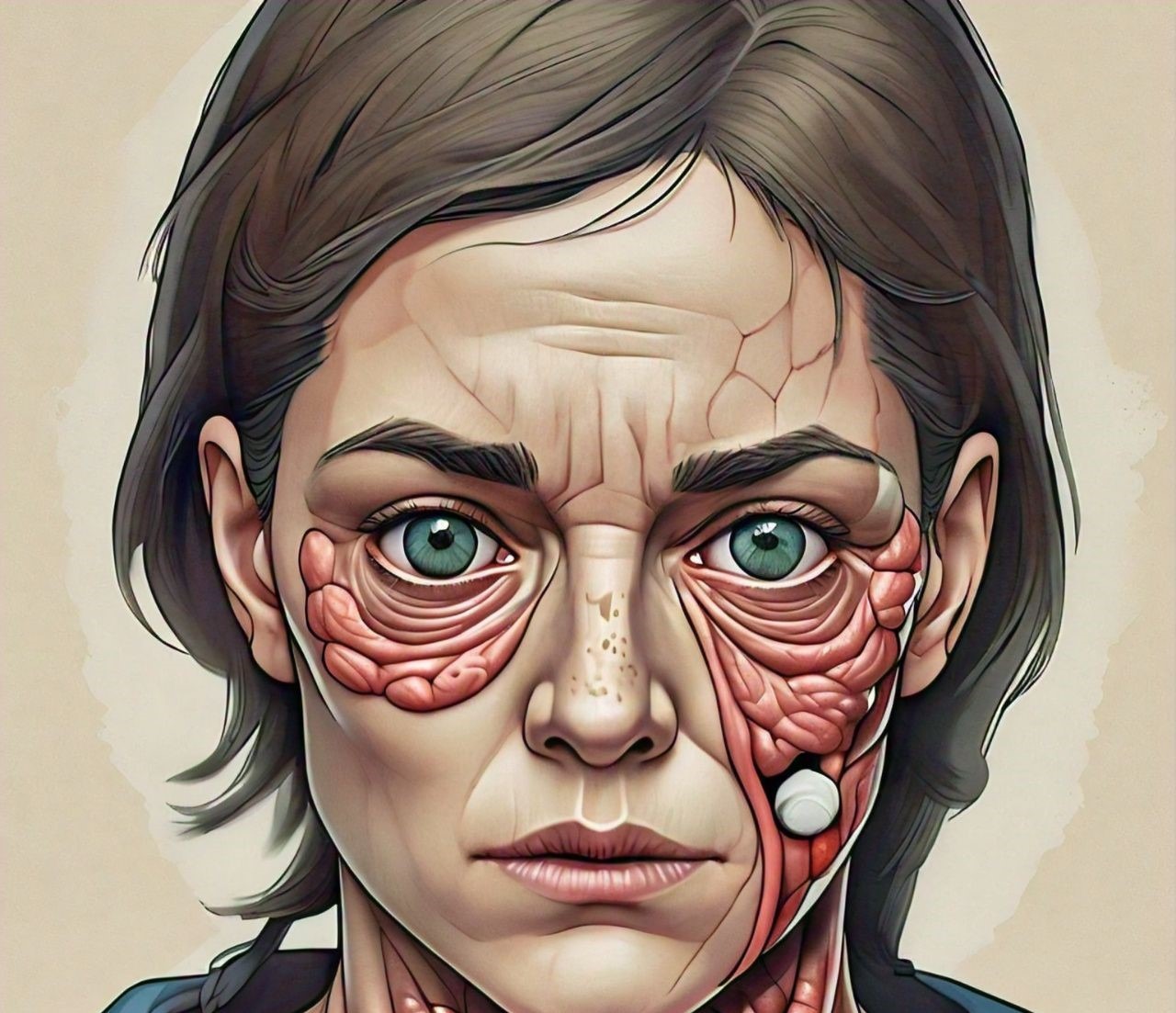
- Graves’ Ophthalmopathy: This condition causes bulging eyes, sensitivity to light, and double vision. It occurs in about 30% of people with Graves’ disease.
- Goiter: The thyroid gland may become enlarged, causing a visible swelling at the base of the neck.
- Pretibial Myxedema: Though rare, this condition causes thick, red skin on the shins and tops of the feet.
How Graves’ Disease Affects Your Body
Graves’ disease impacts various systems in the body, particularly because the thyroid hormones regulate metabolism, heart rate, and body temperature.
Thyroid Hormones and Your Metabolism
The thyroid hormones (T3 and T4) play a crucial role in controlling your body’s metabolism. In Graves’ disease, these hormones are overproduced, causing the body’s metabolism to speed up. This can lead to:
- Rapid Weight Loss: As your metabolism speeds up, your body burns calories faster, often leading to unintended weight loss.
- Increased Appetite: Despite losing weight, many people with Graves’ disease feel constantly hungry and eat more than usual.
Impact on Mental and Emotional Health
Graves’ disease can also affect mental and emotional well-being. The excess thyroid hormone can cause:
- Anxiety: Many people with Graves’ disease experience intense anxiety or panic attacks.
- Mood Swings: Sudden changes in mood, irritability, and short temper are common.
- Depression: Over time, the emotional strain of Graves’ disease can lead to depression, especially if left untreated.
Long-term Health Effects of Untreated Graves’ Disease
If Graves’ disease is not treated, it can lead to severe complications:
- Osteoporosis: The excess thyroid hormone can interfere with calcium absorption, leading to weakened bones.
- Heart Disease: An overactive thyroid can increase heart rate and blood pressure, leading to potential heart problems.
- Thyroid Storm: This rare but life-threatening condition occurs when the thyroid becomes overactive, leading to dangerously high levels of thyroid hormones.
How to Differentiate Graves’ Disease from Other Conditions
Because many of the symptoms of Graves’ disease can mimic other conditions, it’s important to understand the key differences.
Is it Hyperthyroidism or Graves’ Disease?
Graves’ disease is the most common cause of hyperthyroidism, but not all cases of hyperthyroidism are due to Graves’ disease. Other causes include thyroid nodules or thyroiditis. The key distinguishing factor in Graves’ disease is that it is an autoimmune disorder, while hyperthyroidism can have multiple causes.
Graves’ Disease vs. Other Autoimmune Disorders
Graves’ disease shares similarities with other autoimmune disorders like Hashimoto’s thyroiditis, lupus, and rheumatoid arthritis. However, it is unique in its specific attack on the thyroid gland. The symptoms of these conditions may overlap, such as fatigue and joint pain, but Graves’ disease will specifically affect thyroid hormone levels.
What Other Conditions Mimic the Symptoms of Graves’ Disease?
Conditions such as anxiety disorders, menopause, or chronic stress can mimic some of the symptoms of Graves’ disease, such as weight loss, anxiety, and irritability. However, thyroid-specific symptoms like goiter and bulging eyes are unique to Graves’ disease.
Diagnosing Graves’ Disease
When Should You See a Doctor?
If you notice any combination of the symptoms mentioned above, especially if you have a family history of thyroid issues, it’s important to see a doctor. Early diagnosis can prevent complications and improve long-term outcomes.
How is Graves’ Disease Diagnosed?
Diagnosis usually involves several tests to confirm an overactive thyroid:
- Blood Tests: These measure levels of thyroid-stimulating hormone (TSH), T3, and T4. In Graves’ disease, TSH is usually low, while T3 and T4 are elevated.
- Antibody Tests: The presence of thyroid-stimulating immunoglobulin (TSI) in the blood confirms that the thyroid is being overstimulated by the immune system.
- Radioactive Iodine Uptake Test: This test measures how much iodine the thyroid absorbs. A high uptake indicates hyperthyroidism.
- Thyroid Scan: A thyroid scan helps to visualize the structure and size of the thyroid, confirming the presence of a goiter or nodules.
The Role of Endocrinologists
Endocrinologists are specialists who focus on disorders of the endocrine system, including the thyroid. If you are diagnosed with Graves’ disease, your primary care physician may refer you to an endocrinologist for specialized care and long-term management.
Treatment Options for Graves’ Disease
How is Graves’ Disease Treated?
Graves’ disease treatment aims to manage hyperthyroidism and reduce the symptoms of an overactive thyroid. There are several treatment options available, and the choice depends on the severity of the condition, the patient’s age, and other factors like overall health.
1. Anti-Thyroid Medications
Anti-thyroid medications, such as methimazole and propylthiouracil (PTU), help reduce the amount of thyroid hormones produced by the thyroid gland. These drugs are often the first line of treatment, especially in mild cases of Graves’ disease or when other treatments are not suitable.
- How they work: These medications block the thyroid from absorbing iodine, which is necessary for hormone production.
- Duration: Patients may take these medications for 1-2 years. In some cases, remission can be achieved, but the disease may relapse.
- Side effects: Side effects can include liver issues, rashes, and a rare reduction in white blood cells.
2. Radioactive Iodine Therapy
Radioactive iodine therapy (RAI) is a common and highly effective treatment for Graves’ disease. The patient ingests a small dose of radioactive iodine, which is absorbed by the thyroid gland. Over time, the radiation destroys overactive thyroid cells, reducing hormone production.
- Effectiveness: RAI is successful in most cases, leading to long-term management of hyperthyroidism. However, it often results in hypothyroidism (underactive thyroid), requiring lifelong thyroid hormone replacement therapy.
- Procedure: The treatment is done on an outpatient basis, and patients may need to avoid close contact with others for a short time after treatment due to the radiation.
3. Thyroid Surgery (Thyroidectomy)
In more severe cases, or when other treatments are not successful, a thyroidectomy may be performed. This surgical procedure involves the removal of part or all of the thyroid gland.
- Partial vs Total Thyroidectomy: A partial thyroidectomy removes only part of the thyroid, while a total thyroidectomy removes the entire gland. Most patients with total thyroidectomy will require lifelong thyroid hormone replacement therapy.
- Risks: Surgery carries risks, including damage to the vocal cords or parathyroid glands (which regulate calcium levels in the body).
4. Beta-Blockers
While beta-blockers do not address the underlying hyperthyroidism, they are often prescribed to manage symptoms like rapid heart rate, tremors, and anxiety.
- How they work: Beta-blockers, such as propranolol, work by blocking the effects of thyroid hormones on the body, reducing symptoms.
- Short-term use: They are usually used in conjunction with other treatments or while waiting for other therapies (like anti-thyroid drugs or RAI) to take effect.
5. Lifestyle and Home Remedies
Managing Graves’ disease also involves certain lifestyle changes and home remedies that can help alleviate symptoms and support overall health:
- Dietary adjustments: Eating a well-balanced diet rich in calcium and vitamin D can help maintain bone health, as hyperthyroidism can lead to bone thinning.
- Stress management: Since stress can exacerbate symptoms, practices like yoga, meditation, and mindfulness can be beneficial.
- Regular check-ups: Ongoing monitoring of thyroid hormone levels is crucial to ensure the treatment is effective and to adjust medications as necessary.
Potential Complications of Graves’ Disease
Graves’ disease, if left untreated, can lead to serious health complications, some of which can be life-threatening. Understanding these risks emphasizes the importance of early detection and treatment.
1. Graves’ Ophthalmopathy
Graves’ ophthalmopathy, also known as thyroid eye disease, affects about 30% of people with Graves’ disease. It occurs when the immune system attacks the tissues and muscles around the eyes, leading to inflammation and swelling.
- Symptoms: Eye discomfort, bulging eyes (exophthalmos), double vision, and light sensitivity.
- Treatment: Mild cases can be managed with lubricating eye drops, while more severe cases may require corticosteroids, radiation therapy, or surgery to relieve pressure on the optic nerve.
2. Thyroid Storm
A thyroid storm is a rare but life-threatening complication of untreated or poorly controlled hyperthyroidism. It occurs when thyroid hormone levels rise dramatically, leading to severe symptoms such as:
- Symptoms: Rapid heart rate, high fever, confusion, vomiting, and even heart failure.
- Emergency treatment: Immediate medical attention is required. Treatment usually involves intravenous fluids, medications to reduce thyroid hormone levels, and beta-blockers to manage heart rate.
3. Osteoporosis
Hyperthyroidism can lead to bone thinning or osteoporosis, as it increases the rate at which the body breaks down bone tissue. This can lead to an increased risk of fractures.
- Prevention: Ensuring adequate calcium and vitamin D intake, along with weight-bearing exercises, can help protect bone health.
4. Heart Issues
Graves’ disease can put significant strain on the heart due to increased heart rate and high blood pressure, which can lead to conditions like atrial fibrillation and heart failure if left untreated.
- Monitoring: Regular monitoring of heart health and managing hyperthyroidism can help reduce these risks.
Can Graves’ Disease Be Prevented?
There is currently no known way to prevent Graves’ disease, as it is largely determined by genetic and immune system factors. However, early diagnosis and treatment can significantly reduce the risk of complications and improve quality of life.
- Risk factors: A family history of autoimmune diseases, being female, and certain lifestyle factors (like smoking) can increase the risk of developing Graves’ disease.
- Managing risk: While prevention may not be possible, maintaining a healthy lifestyle, managing stress, and regular medical check-ups can help catch the disease early.
Living with Graves’ Disease
Living with Graves’ disease can be challenging, but with proper treatment and lifestyle adjustments, most people can manage their symptoms and lead fulfilling lives. It’s essential to work closely with healthcare providers to tailor treatment to individual needs.
1. Monitoring and Follow-Up
Regular follow-up visits with an endocrinologist are crucial for monitoring thyroid hormone levels, adjusting medications, and preventing potential complications.
2. Support Networks
Joining support groups, either online or in-person, can provide emotional support and practical advice for managing daily life with Graves’ disease.
3. Mental Health
Since Graves’ disease can affect mental well-being, it’s important to prioritize mental health. Seeking counseling or therapy can be beneficial in managing anxiety, depression, or mood swings associated with the condition.
Conclusion
Graves’ disease is a complex autoimmune disorder that requires careful management and treatment. By recognizing the early symptoms of Graves’ disease, seeking prompt medical attention, and following the prescribed treatment plan, individuals can significantly reduce the risks of complications and improve their quality of life.
Understanding the treatment options—from anti-thyroid medications to radioactive iodine therapy and surgery—allows patients and their healthcare providers to make informed decisions about managing this condition.
With ongoing monitoring, support, and a proactive approach to health, living with Graves’ disease becomes manageable, allowing individuals to continue leading healthy and fulfilling lives.
For more information on fitness and health, check out these resources:
Explore more articles on our site:
- How to Increase Running Stamina for Beginners at Home
- What Happens if You Don’t Get Enough Sleep Consistently: Effects and Solutions
- The Ultimate Guide to Healthy Living in 2024
- The Future of Artificial Intelligence: What to Expect
- Unlocking the Potential of Chat GPT Software: Revolutionizing AI Conversations
- Best Sleeping Position for Peripheral Artery Disease [New 2024]
- How to Increase Running Stamina for Beginners at Home
- 5 New Inner Thigh Exercises for Men and Women